Amy Diagnosed at age 35
"We have been together for 25 years, married for 15, and this whole cancer thing has actually strengthened our love and made us appreciate even more the most important thing in life: family."
I had my first scheduled baseline mammogram in July 2002 at age 35 and everything was normal. Then in February 2003 my husband found a small lump. (I have learned since that spouses find the majority of breast abnormalities) I called my gynecologist to report it at the insistence of my friends. My annual exam was already scheduled for three months later but she wanted me to come in right then to have it checked out. From what I’ve heard and read here on the YSC discussion boards, she acted very conservatively compared to some of her peers when dealing with a young, healthy, non-smoker with no family history of breast cancer. The breast specialist I saw sent me for a repeat mammogram and an ultrasound but assured me that 9 out of 10 of these lumps turn out to be benign. From there I was sent to see a general surgeon for a biopsy but still believed there was nothing to worry about.
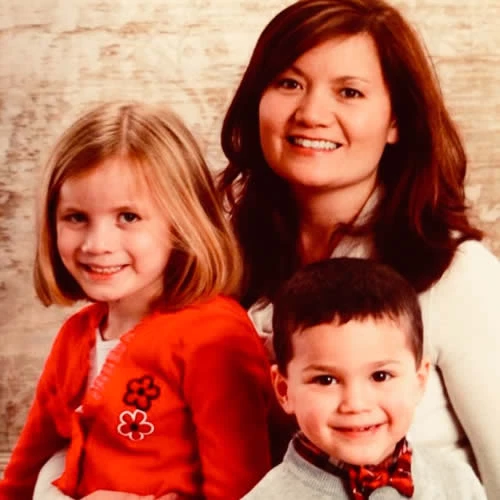
Oh, that fine needle aspiration was the most painful procedure I’ve endured since childbirth! The surgeon sent my sample down to the lab immediately and I sat in the waiting room with my mom planning where we were going for dinner. In retrospect, I know that was the last truly carefree moment of my life. My husband had not come with me to this appointment because we didn’t for a second think this could be anything serious. The doctor called me back in and delivered the crushing news that this was indeed breast cancer, and that I would need surgery and possibly chemotherapy. That’s about all I heard. When he kindly asked me if I had any children, I lost it. All I heard was “you are going to die and won’t be around to see your two sons grow up.” My God, they are only 7 and 5! I’m a stay-at-home mom and they depend on me so completely! This cannot be happening!
The next few weeks are a blur: bone scans and chest x-rays and second opinions. I ended up switching to a breast cancer surgeon at Ohio State University’s James Cancer Hospital. I had a lumpectomy in March but the tumor, 1.6 cm, had branched off under my nipple and he couldn’t get clear margins so I had to then have a mastectomy two weeks later. My sentinel node had microscopic cancer cells in it so he removed all 14 lymph nodes but only the sentinel node was positive. I chose to have immediate reconstruction with a saline tissue expander.
My chemotherapy treatments began in late May with Adriamycin/Cytoxin. My hair fell out right on schedule 2 weeks later. As my husband cut my hair to a GI Jane-like buzz, I sobbed for only the second time since my diagnosis. I can’t say why, but losing my hair was more traumatic than losing my breast! I slogged through the summer in bandanas and baseball caps and tolerated the chemo like a trouper: no nausea or vomiting, and not much fatigue. Actually, if I’d had hair, no one would have known I was a cancer patient!
I am an Avon representative and I kept my business going with no gaps. My husband and friends delivered my brochures and orders and I could do the rest from home. I had also worked one night a week as a waitress but I took 6 months off from that job because of the late nights and the strenuous nature of the job. Because of my her2neu 3+ status, I signed up for a clinical trial for the drug Herceptin, which was then used only for metastatic disease. Researchers think it may also be effective in preventing metastasis. In August I learned that I was randomized to the non-Herceptin arm of the trial, which meant I would receive only the standard therapy: 12 weekly Taxol treatments after the Adriamycin/Cytoxin. My husband was greatly disappointed that I was not allowed to take Herceptin anyway – at the time, it was not available off trial to any patients but Stage IV. I was relieved though – I was not looking forward to 77 more weekly infusions!
A word of suggestion to anyone considering a port: do it! I did not have one put in because I didn’t think I needed to “save” my veins. I thought that meant “save me from the pain of the IV insertions,” but what it really means is “save the actual veins from the chemical assault of the chemo drugs.” My veins are now rock hard and tight and almost impossible to locate for blood draws. Before my last reconstructive surgery, the anesthesiologist tried without luck to put an IV in my hand, arm, both feet and neck before finally using my jugular vein!
There was a time when every ache and pain had me assuming it was a recurrence. But I had to be around to raise my boys. They needed me, and still do. I plan to see my older son kick butt on his high school football team. And I plan to watch my younger son earn a state championship in wrestling. I'm now working a third part-time job - substitute teacher. Life is great and there really was a light at the end of my dark tunnel.
In 2003, my husband informed me that he just can’t do it alone. He has truly been my rock! He has never faltered in his love or desire for me through all of this. I could not ask for more unequivocal support from a spouse. We have been together for 25 years, married for 15, and this whole cancer thing has actually strengthened our love and made us appreciate even more the most important thing in life: family. Best wishes to all who read this!
If this is your story and you'd like to update it, please email us at [email protected].
Are you a survivor, spouse, friend, or caretaker with a story to tell? We'd love to hear from you.